Many people with IBD may require a surgery at some point in their lifetimes. Surgery should not be considered a “failure of treatment” – as in many cases, surgery may be the best option for the person. In some cases, medications may be started “too late” in the disease course, after complications (e.g. strictures) have already developed – in these cases, surgery AND medications together may be the best option.
Resection is a surgery to remove a section of the intestines. Small bowel resection means a piece of small bowel is resected. Pieces of the large bowel (colon) can also be resected if needed. Common parts of the intestine to be resected are strictures, diseased areas, areas with pre-malignancy. People with Crohn’s disease may have history of multiple small bowel resections due to removal of strictures, fistulizing areas, inflamed areas.
For more information on resections for Crohn’s disease, please view this short video.
Strictures as described before are fixed narrowings of the bowel due to fibrosis or scarring from previous inflammation. Strictures are most commonly found in the small bowel in Crohn’s patients. Strictures that are causing problems (obstructions or blockages if too narrow) are often surgically resected, but in some cases they are cut open and sewn up in the other direction (plasty) to keep them open.
Colectomy is a surgery to remove the colon. Hemicolectomy means only half the colon is removed. Subtotal colectomy means most of the colon is removed, but the rectum is left inside. Subtotal colectomy is performed in cases of emergency or if the intent is to have a second surgery to create an internal pouch. Total colectomy means the entire colon including the rectum is removed.
Ostomy refers to the creation of a stoma, or an opening of the intestines to the skin to allow passage of stool. Ostomy can be ileostomy (the ileum exits the skin) or colostomy (the colon exits the skin).
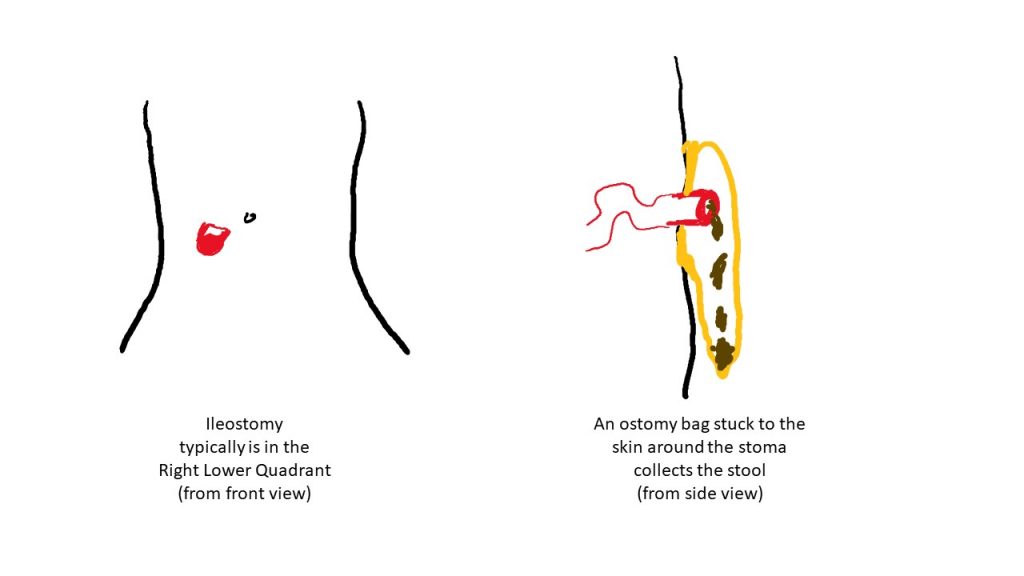
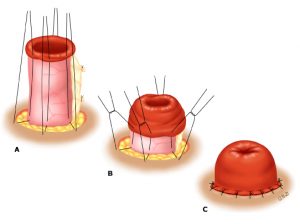
Ostomies can be temporary or permanent. A temporary ileostomy typically is a loop or diversion ostomy, meaning that a loop of intestine is brought out to the skin and everted (turned on itself) to produce the spout. Diversion ostomy is sometimes used to allow the large bowel or perianal disease to heal, as the stool will be passed through the ostomy and not pass through the colon. With a permanent ileostomy or end-ileostomy, the stoma creation is permanent, meaning no plan to reconnect and reverse the stoma. To create a stoma, surgeons will pull the end of the small intestine through the surgical opening, out of the abdomen, turn it on itself (evert), and suture – so that it protrudes out like a spout – this allows the intestinal feces and content to exit and flow away from the stoma/skin connection.
People who had colectomy often will have an internal pouch created. This is most often the case in people with ulcerative colitis, rarely do surgeons create pouch in Crohn’s disease. The most common pouch or Ileal Pouch Anal Anastomosis (IPAA) is the J-pouch, called J due to the shape. The pouch is created from the small bowel and eventually acts as a reservoir for stool.
Watch the Toronto Video Atlas of Surgery (TVASurg) Patient education video for more information on surgery options for ulcerative colitis.
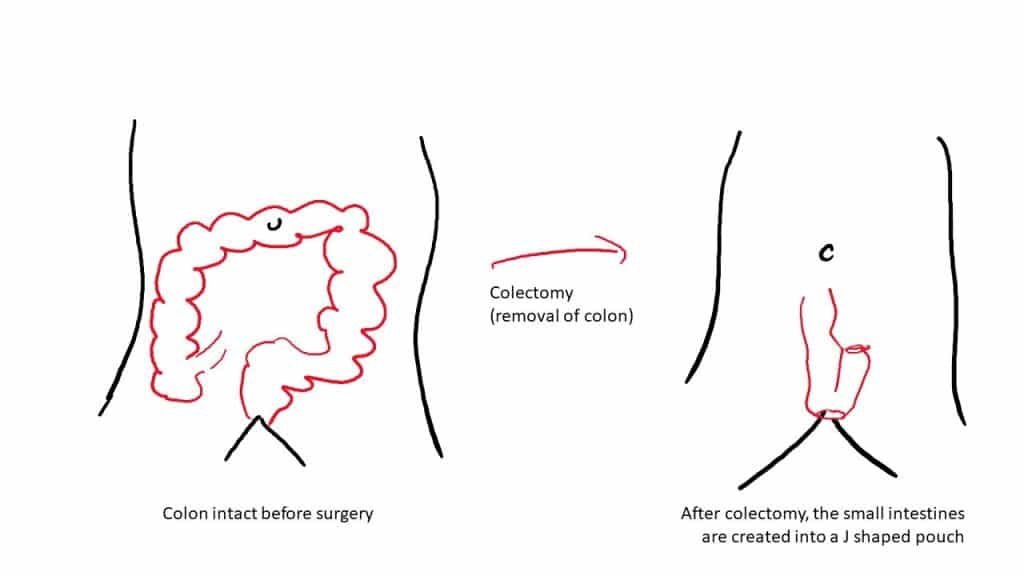
People with an internal pouch still have bowel motions about 4 to 6 times a day, but the disease burden is removed. Some people do develop inflammation of the pouch or “pouchitis” which can be treated with antibiotics and other medications. Although colectomy and pouch creation is considered a “cure” for ulcerative colitis, some people may develop Crohns disease of the pouch, in which case immunosuppressants and biologics are often used to treat the disease.
Incision and drainage or I and D refers to a small surgery where the skin above an abscess is cut or incised open, and the abscess drained. I and D are done frequently to treat perianal abscesses.